Credentialing
Medenar Healthcare is a well-known supplier of healthcare services and medical billing.
Credentialing
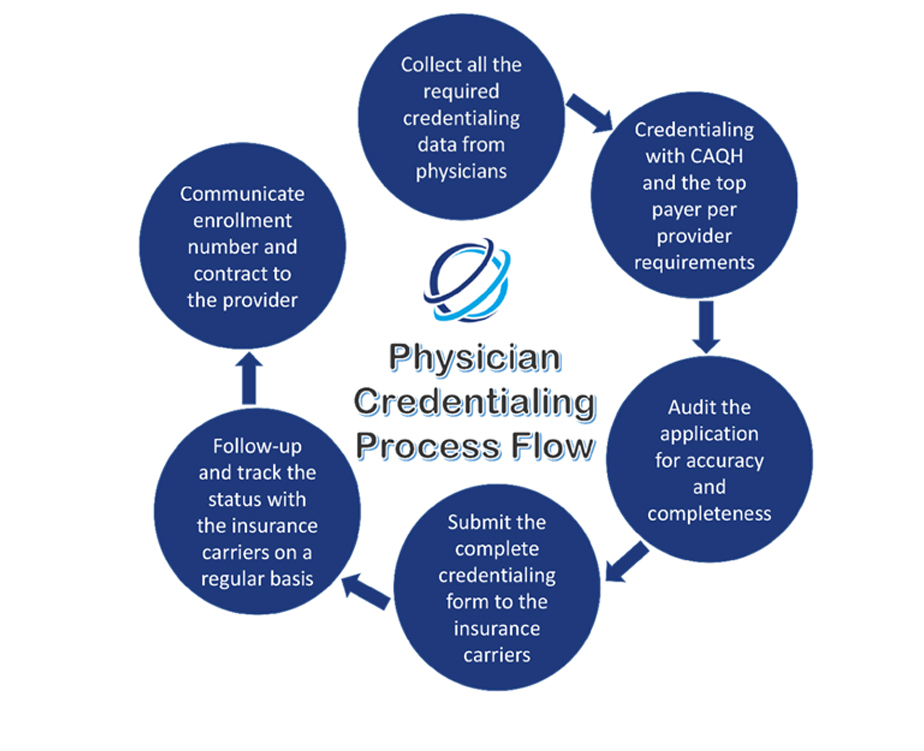
Physician credentialing and provider enrollment services is a process of enrolment and attestation that a physician is part of a Payer’s network and authorized to provide services to patients who are members in the Payer’s plans. Credentialing verifies that a physician meets standards as determined by the Payer by reviewing such items as the individual’s license, experience, certification, education, training, affiliations, malpractice & adverse clinical occurrences and clinical judgment.
Effective provider credentialing services are the absolute necessity for better performance of the practice. Without proper enrolment, payments can be delayed or refused by the insurance carriers, even if the physician is able to provide services that are competent and medically necessary.